Liver Fibrosis: The Basics
Liver fibrosis, also known as hepatic fibrosis, is the excessive accumulation of scar tissue (extracellular matrix proteins, collagen) that occurs in most chronic liver diseases.1 Advanced stages of liver fibrosis lead to debilitating outcomes, including cirrhosis (characterized by degeneration of cells, thickening of tissue, and inflammation), liver failure, and portal hypertension. Liver cirrhosis is a leading cause of liver disease-related deaths worldwide and substantial research is dedicated towards understanding targetable mechanisms for treatment.2
Several factors can lead to an increased risk of liver fibrosis. This includes viral infections, alcoholism, and toxins. The pathogenesis of liver fibrosis is dynamic and complex,3 considering the liver’s ability to regenerate. In response to injury, inflammation triggers a wound-healing process aimed at mitigating tissue damage; however, it also results in the accumulation of scar tissue. Progression towards the end-stage of liver fibrosis, or cirrhosis, results in severe architectural and vascular disruption. Although liver fibrosis is a counter-regulatory response to liver damage, without intervention, it ultimately leads to cirrhosis and liver cancer.
Understanding the mechanisms and pathways that regulate liver fibrosis is critical for early detection and effective treatment to reverse fibrosis. With the advent of new systems biology approaches, metabolomics has emerged as an important tool for providing key insights into disease progression and diagnosis.
Challenges in Liver Fibrosis Research
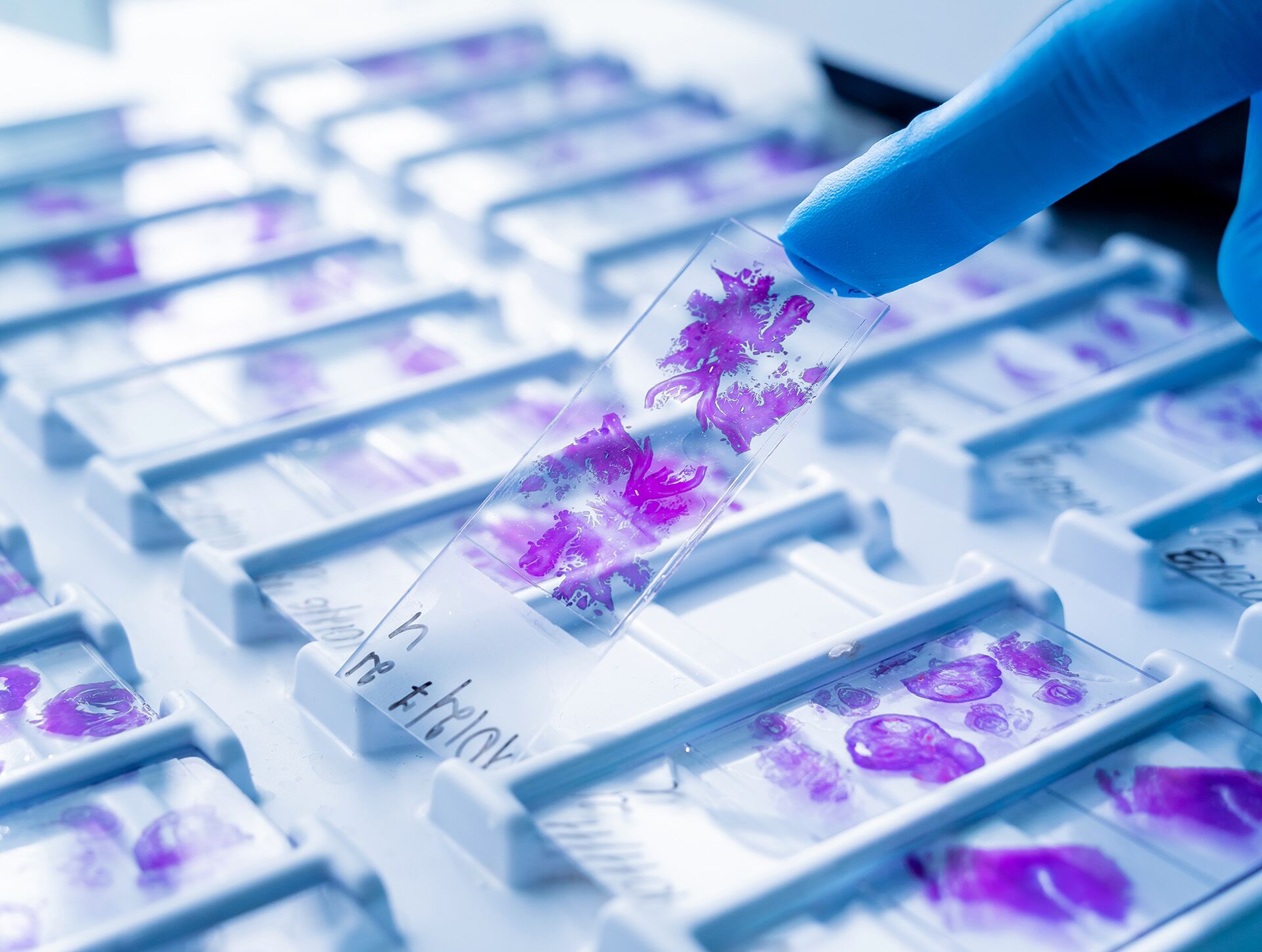
The current gold standard for evaluating liver fibrosis is liver biopsy. However, this procedure is invasive, carries considerable risks, and increases sampling errors and variability.4 Additionally, it is time-consuming and often fails to provide a comprehensive systems-level perspective on the mechanisms and pathways associated with liver fibrosis. Existing biomarkers lack specificity and have limited applicability, highlighting the urgent need for better tools that can accurately and non-invasively detect biomarkers during the early stages of liver fibrosis.
The effective treatment of liver diseases relies on an accurate assessment of the extent of fibrosis. Current research efforts focus on deeper investigations into inflammation and require improved techniques for the comprehensive evaluation of inflammation, liver damage, and associated metabolite markers with enhanced sensitivity and accuracy.
Insights Gained from Metabolomics
The pathogenesis of liver fibrosis is closely linked to metabolic processes, leading to a surge in research investigating metabolites as biomarkers for liver fibrosis.5 Metabolomics has played a crucial role in providing valuable insights into potential biomarkers that can be detected in the early stages of fibrosis with high sensitivity and accuracy.
Recognizing the limitations of current diagnostic and tracking methods for liver fibrosis, a group of researchers utilized serum and urine metabolomics to study a rat model of liver fibrosis.6 Their findings identified significant changes in nine urine metabolites and ten serum metabolites during the early stages of liver fibrosis. These included perturbations of tryptophan, valine, leucine, isoleucine, and citrate (TCA) cycle metabolites as well as sphingolipid and glycerophospholipid metabolites at the onset of fibrosis. Interestingly, the conversion of tryptophan to kynurenic acid (i.e., Kyn pathway) has been shown to be associated with inflammation and oxidative stress that then contributes to tissue fibrosis.7 Collectively, these results provide promising early-stage biomarkers that can be targeted for treatment.
In another study, researchers examined humans with non-alcoholic fatty liver disease (NAFLD) using metabolomics to gain critical insights into liver fibrosis biomarkers.8 Their findings revealed that out of 652 analyzed metabolites, 32 were associated with advanced fibrosis. Among the top ten metabolites, eight lipids (5alpha-androstan-3beta monosulfate, pregnanediol-3-glucuronide, androsterone sulfate, epiandrosterone sulfate, palmitoleate, dehydroisoandrosterone sulfate, 5alpha-androstan-3beta disulfate, glycocholate), one amino acid (taurine) and one carbohydrate (fucose) were shown to be excellent for detecting the presence of advanced fibrosis. Notably, all of these top ten metabolites had an area under the receiver operating characteristic curve (AUROC) higher than the FIB-4 index (noninvasively estimates liver scarring) and the NAFLD Fibrosis Score (NFS) for detecting advanced liver fibrosis, demonstrating that these metabolites could be more predictive of advanced fibrosis than current fibrosis scoring systems.
Figure 1. Metabolite biomarkers found in individuals at different liver fibrosis stages.5
Metabolon’s Liver Fibrosis Discovery Panel
Metabolon has leveraged advances in metabolomics to address the needs of researchers, clinicians, and doctors. The application of metabolomics, as demonstrated above, has yielded significant insights into discovering new biomarkers and identifying novel therapeutic targets for early-stage interventions.
Metabolon’s Liver Fibrosis Discovery Panel is uniquely positioned to capture and track liver disease phenotypes from a systems level perspective. Designed to measure relative quantitative changes for 97 metabolites, including lipids (e.g., 5alpha-androstan-3beta monosulfate), amino acids (e.g., taurine), and carbohydrates (e.g., fucose), across various biological pathways, the Liver Fibrosis Discovery panel is non-invasive, sensitive, and comprehensive. Contact us to learn more.
Liver Fibrosis Discovery Panel
The Liver Fibrosis Discovery Panel will provide deeper insights for researchers and thereby help them address key factors in liver fibrosis, including mechanistic insights, personalized medicine, and drug discovery, and testing.
References
- Bataller R, and Brenner DA. Liver fibrosis. J Clin Invest 2005;115(2):209–218.
- Lozano R, Naghavi M, Foreman K et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380(9859):2095–2128.
- Schuppan D and Kim YO. Evolving therapies for liver fibrosis. J Clin Invest 2013;123(5):1887–1901.
- Huang H, Sun Z, Pan H, et al. Serum metabolomic signatures discriminate early liver inflammation and fibrosis stages in patients with chronic hepatitis B. Sci Rep 2016;6:30853.
- Kim, HY. Recent advances in nonalcoholic fatty liver disease metabolomics. Clin Mol Hepatol 2021;27(4):553–559.
- Chang H, Meng HY, Liu SM et al. Identification of key metabolic changes during liver fibrosis progression in rats using a urine and serum metabolomics approach. Sci Rep 2017;7(1):11433.
- Chen H, Cao,G, Chen DQ et al. Metabolomics insights into activated redox signaling and lipid metabolism dysfunction in chronic kidney disease progression. Redox Biol 2016;10:168–178.
- Caussy C, Ajmera VH, Puri P et al. Serum metabolites detect the presence of advanced fibrosis in derivation and validation cohorts of patients with non-alcoholic fatty liver disease. Gut 2019;68(10):1884–1892.